..... Click the link for more information. ). Since the heart can pump blood into the large arteries more quickly than it can be absorbed and released by the tiny arterioles and capillaries, considerable inner pressure always exists in the arteries. The contraction of the heart (systole) causes the blood pressure to rise to its highest point, and relaxation of the heart (diastole) brings the pressure down to its lowest point.
Blood pressure is strongest in the aorta, where the blood leaves the heart. It diminishes progressively in the smaller blood vessels and reaches its lowest point in the veins (see circulatory system circulatory system, group of organs that transport blood and the substances it carries to and from all parts of the body. The circulatory system can be considered as composed of two parts: the systemic circulation, which serves the body as a whole except for the
..... Click the link for more information. ). Blood pressure manifests itself dramatically when an artery is severed or pierced and the blood (under pressure) ejects in spurts.
Since blood pressure varies in different arteries, the pressure in the brachial artery of the forearm serves as a standard. A sphygmomanometer measures blood pressure in millimeters of mercury; blood pressure gauges that do not use mercury also produce readings that are expressed in terms of millimeters of mercury. Normal blood pressure readings for healthy young people should be below 120 mm for systolic pressure and 80 mm for diastolic pressure, commonly written as 120/80 and read as "one-twenty over eighty." With age, and the constriction of the small arteries and then the larger ones, blood pressure increases, so that at 50 years, a person may typically have a systolic pressure between 140 and 150, and a diastolic pressure of about 90.
Blood pressure- See Hypertension for more information about recognition and treatment of high blood pressure.
Blood pressure refers to the force exerted by circulating blood on the walls of blood vessels, and constitutes one of the principal vital signs. The pressure of the circulating blood decreases as blood moves through arteries, arterioles, capillaries, and veins; the term blood pressure generally refers to arterial pressure, i.e., the pressure in the larger arteries, arteries being the blood vessels which take blood away from the heart. Arterial pressure is most commonly measured via a sphygmomanometer, which uses the height of a column of mercury to reflect the circulating pressure (see Non-invasive measurement). Blood pressure values are reported in either kilopascals (kPa) or in millimetres of mercury (mmHg), despite the fact that many modern vascular pressure devices no longer use mercury.
The systolic arterial pressure is defined as the peak pressure in the arteries, which occurs near the beginning of the cardiac cycle; the diastolic arterial pressure is the lowest pressure (at the resting phase of the cardiac cycle). The average pressure throughout the cardiac cycle is reported as mean arterial pressure; the pulse pressure reflects the difference between the maximum and minimum pressures measured.
Typical values for a resting, healthy adult human are approximately 120 mmHg (16 kPa) systolic and 80 mmHg (11 kPa) diastolic (written as 120/80 mmHg, and spoken as "one twenty over eighty") with large individual variations. These measures of arterial pressure are not static, but undergo natural variations from one heartbeat to another and throughout the day (in a circadian rhythm); they also change in response to stress, nutritional factors, drugs, or disease. Hypertension refers to arterial pressure being abnormally high, as opposed to hypotension, when it is abnormally low. Along with body temperature, blood pressure measurements are the most commonly measured physiological parameters.
Measurement
Arterial pressures can be measured invasively (by penetrating the skin and measuring inside the blood vessels) or non-invasively. The former is usually restricted to a hospital setting.
Non-invasive measurement
The non-invasive auscultatory (from the Latin for listening) and oscillometric measurements are simpler and quicker than invasive measurements, require less expertise in fitting, have virtually no complications, and are less unpleasant and painful for the patient. However, non-invasive measures may yield somewhat lower accuracy and small systematic differences in numerical results. Non-invasive measurement methods are more commonly used for routine examinations and monitoring.
Palpation methods
A minimum systolic value can be roughly estimated without any equipment by palpation, most often used in emergency situations. Palpation of a radial pulse indicates a minimum blood pressure of 80 mmHg (11 kPa), a femoral pulse indicates at least 70 mmHg (9.3 kPa), and a carotid a minimum of 60 mmHg (8.0 kPa). However, one study indicated that this method was not accurate enough and often overestimated patient's systolic blood pressure.[1] A more accurate value of systolic blood pressure can be obtained by with a sphygmomanometer and palpating for when a radial pulse returns.[2] Because a diastolic pressure cannot be obtained by this method, blood pressures obtained by palpation are noted as "
Auscultatory methods
The auscultatory method uses a stethoscope and a sphygmomanometer. This comprises an inflatable (Riva-Rocci) cuff placed around the upper arm at roughly the same vertical height as the heart, attached to a mercury or aneroid manometer. The mercury manometer, considered to be the gold standard for arterial pressure measurement, measures the height of a column of mercury, giving an absolute result without need for calibration, and consequently not subject to the errors and drift of calibration which affect other methods. The use of mercury manometers is often required in clinical trials and for the clinical measurement of hypertension in high risk patients, such as pregnant women.
A cuff of appropriate size is fitted and inflated manually by repeatedly squeezing a rubber bulb until the artery is completely occluded. Listening with the stethoscope to the brachial artery at the elbow, the examiner slowly releases the pressure in the cuff. When blood just starts to flow in the artery, the turbulent flow creates a "whooshing" or pounding (first Korotkoff sound). The pressure at which this sound is first heard is the systolic blood pressure. The cuff pressure is further released until no sound can be heard (fifth Korotkoff sound), at the diastolic arterial pressure. Sometimes, the pressure is palpated (felt by hand) to get an estimate before auscultation.
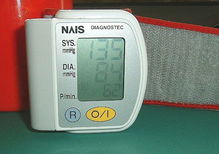
Oscillometric methods
Oscillometric methods are sometimes used in the long-term measurement and sometimes in general practice. The equipment is functionally similar to that of the auscultatory method, but with an electronic pressure sensor (transducer) fitted in to detect blood flow, instead of using the stethoscope and the expert's ear. In practice, the pressure sensor is a calibrated electronic device with a numerical readout of blood pressure. To maintain accuracy, calibration must be checked periodically, unlike the inherently accurate mercury manometer. In most cases the cuff is inflated and released by an electrically operated pump and valve, which may be fitted on the wrist (elevated to heart height), although the upper arm is preferred. They vary widely in accuracy, and should be checked at specified intervals and if necessary recalibrated.
Oscillometric measurement requires less skill than the auscultatory technique, and may be suitable for use by untrained staff and for automated patient home monitoring.
The cuff is inflated to a pressure initially in excess of the systolic arterial pressure, and then reduces to below diastolic pressure over a period of about 30 seconds. When blood flow is nil (cuff pressure exceeding systolic pressure) or unimpeded (cuff pressure below diastolic pressure), cuff pressure will be essentially constant. It is essential that the cuff size is correct: undersized cuffs may yield too high a pressure, whereas oversized cuffs yields too low a pressure. When blood flow is present, but restricted, the cuff pressure, which is monitored by the pressure sensor, will vary periodically in synchrony with the cyclic expansion and contraction of the brachial artery, i.e., it will oscillate. The values of systolic and diastolic pressure are computed, not actually measured from the raw data, using an algorithm; the computed results are displayed.
Oscillometric monitors may produce inaccurate readings in patients with heart and circulation problems, that include arterial sclerosis, arrhythmia, preeclampsia, pulsus alternans, and pulsus paradoxus.
In practice the different methods do not give identical results; an algorithm and experimentally obtained coefficients are used to adjust the oscillometric results to give readings which match the auscultatory as well as possible.[4] Some equipment uses computer-aided analysis of the instantaneous arterial pressure waveform to determine the systolic, mean, and diastolic points. Since many oscillometric devices have not been validated, caution must be given as most are not suitable in clinical and acute care settings.
The term NIBP, for Non-Invasive Blood Pressure, is often used to describe oscillometric monitoring equipment.
Invasive measurement
Arterial blood pressure (BP) is most accurately measured invasively through an arterial line. Invasive arterial pressure measurement with intravascular cannulae involves direct measurement of arterial pressure by placing a cannula needle in an artery (usually radial, femoral, dorsalis pedis or brachial). This is usually done by an anesthesiologist or surgeon in a hospital.
The cannula must be connected to a sterile, fluid-filled system, which is connected to an electronic pressure transducer. The advantage of this system is that pressure is constantly monitored beat-by-beat, and a waveform (a graph of pressure against time) can be displayed. This invasive technique is regularly employed in human and veterinary intensive care medicine, anesthesiology, and for research purposes.
Cannulation for invasive vascular pressure monitoring is infrequently associated with complications such as thrombosis, infection, and bleeding. Patients with invasive arterial monitoring require very close supervision, as there is a danger of severe bleeding if the line becomes disconnected. It is generally reserved for patients where rapid variations in arterial pressure are anticipated.
Invasive vascular pressure monitors are pressure monitoring systems designed to acquire pressure information for display and processing. There are a variety of invasive vascular pressure monitors for trauma, critical care, and operating room applications. These include single pressure, dual pressure, and multi-parameter (i.e. pressure / temperature). The monitors can be used for measurement and follow-up of arterial, central venous, pulmonary arterial, left atrial, right atrial, femoral arterial, umbilical venous, umbilical arterial, and intracranial pressures.
Vascular pressure parameters are derived in the monitor's microcomputer system. Usually, systolic, diastolic, and mean pressures are displayed simultaneously for pulsatile waveforms (i.e. arterial and pulmonary arterial). Some monitors also calculate and display CPP (cerebral perfusion pressure). Normally, a zero key on the front of the monitor makes pressure zeroing extremely fast and easy. Alarm limits may be set to assist the medical professional responsible for observing the patient. High and low alarms may be set on displayed temperature parameters.
Home monitoring
Up to 25% of patients diagnosed with hypertension do not suffer from it, but rather from white coat hypertension (elevated arterial pressure specifically during medical exams, probably as a result of anxiety). Thus, well-performed, accurate home arterial pressure monitoring can prevent unnecessary anxiety, as well as costly and potentially dangerous therapy in many millions of people worldwide. Home arterial pressure monitoring provides a measurement of a person's arterial pressure at different times and in different environments, such as at home and at work, throughout the day. Home arterial pressure monitoring may assist in the diagnosis of high or low arterial pressure. It may also be used to monitor the effects of medication or lifestyle changes taken to lower or regulate arterial pressure levels.
Automatic self-contained blood pressure monitors are available at reasonable prices, some of which are capable of Korotkoff's measurement in addition to oscillometric methods, enabling irregular heartbeat patients to accurately measure their blood pressure at home, which was not possible using the traditional devices.
The 2003 US Joint National Committee recommends the use of self monitoring of arterial pressure, before considering the more expensive ambulatory monitoring of arterial pressure, to improve hypertension management.[5] Both the Joint National Committee and the 2003 guidelines from the European Society of Hypertension and the European Society of Cardiology suggest that self monitoring might also be used as an alternative to ambulatory monitoring for the diagnosis of white coat hypertension.[6]
A study published in the May 2006 American Journal of Hypertension[7] compared home and ambulatory blood pressure monitoring methods in the adjustment of antihypertensive treatment. The study showed home arterial pressure monitoring is as accurate as a 24 hour ambulatory monitoring in determining arterial pressure levels. Researchers at the University of Turku, Finland studied 98 patients with untreated hypertension. They compared patients using a home arterial pressure device and those wearing a 24-hour ambulatory monitor. Researcher Dr. Niiranen said that, "home blood pressure measurement can be used effectively for guiding anti-hypertensive treatment". Dr. Stergiou added that home tracking of arterial pressure, "is more convenient and also less costly than ambulatory blood pressure monitoring".
A clinical study published in the May 2007 edition of The American Journal of Hypertension[8] compared the accuracy of three different methods of taking arterial pressure in indicating cardiovascular health. The study aim was to assess the accuracy of home blood pressure monitoring (HBP), 24-hour ambulatory blood pressure monitoring (ABP) and arterial pressure readings taken in a doctor’s office (OBP). The arterial pressure tests were compared to the left-ventricular mass index (LVMI). The LVMI was calculated from an echocardiogram of the heart and indicates cardiovascular organ damage, an indicator of arterial pressure. Researchers at The Columbia University Medical Center, New York found that home arterial pressure monitoring, over a ten-week period was a significant independent predictor of LVMI even after adjusting for age, sex and BMI (body mass index). They found that home monitoring over time is a better indicator of cardiovascular health than ambulatory readings or readings taken at the doctors’ office. The value of home monitoring increases over time with a number of measurements taken.
The June 2007 AMNews; Newspaper for America's Physicians[9] released a study which showed arterial pressure readings taken in a doctors office are often unreliable. The American Medical Association newspaper quoted Prof Norman Kaplan from the University of Texas Southwestern Medical Center who said, "Of all the procedures done in a doctor's office, measurement of blood pressure is usually the least well performed but has the most important implications for the care of the patient." The paper explained that arterial pressure readings taken in a Doctors office can be falsely raised or lowered. This can be due to the presence of a Doctor or clinician which results in the patient experiencing white coat hypertension.
The American Heart Association website[10] states, "You may have what's called 'white coat hypertension'; that means your blood pressure goes up when you're at the doctor's office. Monitoring at home will help you measure your true blood pressure and can provide your doctor with a log of blood pressure measurements over time. This is helpful in diagnosing and preventing potential health problems."
Those using home arterial pressure monitoring devices are increasingly also making use of arterial pressure charting software.[11] These charting methods provide print outs for the patients physician and reminders on how often to check arterial pressure.[12][13]
Accuracy of Home Monitoring
The National Heart, Lung and Blood Institute has issued guidelines for taking blood pressure using home monitoring devices.[14] Obtaining an accurate reading requires that the patient should not drink coffee, smoke cigarettes, or engage in strenuous exercise for 30 minutes before taking the reading. For 5 minutes before the test, the patient should be sitting upright in a chair with his or her feet flat on the floor and without any limbs crossed. The arm should be relaxed and kept at heart level during the reading. The blood pressure cuff should always be against bare skin, as readings taken over a shirt sleeve are less accurate. A full bladder may have a small effect on blood pressure readings, so if the urge to urinate exists, the patient should be encouraged to void the bladder before the reading.[15]
Normal Values
While statistically normal values for arterial pressure could be computed for any given population, there is often a large variation from person to person; arterial pressure also varies in individuals from moment to moment. Additionally, the norm of any given population may have a questionable correlation with its general health, thus the relevance of such statistical values is equally questionable. In a study of 100 subjects with no known history of hypertension, an average systolic blood pressure of 112.4 mmHg (14.99 kPa) and an average diastolic pressure of about 64.0 mmHg (8.53 kPa) was found.[16]
In children the observed normal ranges are lower; in the elderly, they are often higher, largely because of reduced flexibility of the arteries. Factors such as age, gender and race influence blood pressure values. Pressure also varies with exercise, emotional reactions, sleep, digestion and time of the day.
In the U.S., the optimal arterial pressure (sometimes referred to as the ‘gold standard’) targets are:[17][18][19]
Levels above 120 mmHg (16 kPa) but below 140 mmHg (19 kPa) in systolic pressure, or above 80 (11 kPa) but below 95 mmHg (13 kPa) in diastolic pressure, are referred to as "prehypertensive" and often progress to frankly hypertensive levels. However studies already extant reveal that there are fewer complications at, e.g., 115 mmHg (15 kPa) systolic than 120 mmHg (16 kPa), and in fact arterial pressure is a continuum with decreasing pathology associated with lower levels to well within the current "optimum" range. The risk of cardiovascular disease increases progressively throughout the range of arterial pressure, beginning at 115/75 mm Hg.[20] "Some data indicates that 115/75 mm Hg should be the gold standard. Once arterial pressure rises above 115/75 mm Hg, the risk of cardiovascular disease begins to increase. Prehypertension is now considered to be a systolic pressure ranging from 120 to 139 or a diastolic pressure ranging from 80 to 89." (Excerpts from Mayo Clinic website). In the past, hypertension was only diagnosed if secondary signs of high arterial pressure were present, along with a prolonged high systolic pressure reading over several visits. In the US, this reactive stance has been soundly rejected in the light of recent evidence.
In the UK, mirroring abandoned earlier US practice, nursing students continue to be taught that their patients’ readings should be considered ‘normal’ if in the range:
Clinical trials demonstrate that people who maintain arterial pressures at the low end of these pressure ranges have much better long term cardiovascular health. The principal medical debate concerns the aggressiveness and relative value of methods used to lower pressures into this range for those who do not maintain such pressure on their own. Elevations, more commonly seen in older people, though often considered normal, are associated with increased morbidity and mortality. The clear trend from double blind clinical trials (for the better strategies and agents) demonstrates that lower arterial pressure correlates with lower rates of disease.
Physiology
The mean arterial pressure (MAP) is the average pressure measured over one complete cardiac cycle.
The up and down fluctuation of the arterial pressure results from the pulsatile nature of the cardiac output. The pulse pressure is determined by the interaction of the stroke volume versus the resistance to flow in the arterial tree.
The larger arteries, including all large enough to see without magnification, are low resistance (assuming no advanced atherosclerotic changes) conduits with high flow rates that generate only small drops in pressure. For instance, with a subject in the supine position, blood travelling from the heart to the toes typically only experiences a 5 mmHg (0.67 kPa) drop in mean pressure.
Modern physiology developed the concept of the vascular pressure wave (VPW). This wave is created by the heart during the systole and originates in the ascending aorta. Much faster than the stream of blood itself, it is then transported through the vessel walls to the peripheral arteries. There the pressure wave can be palpated as the peripheral pulse. As the wave is reflected at the peripheral veins it runs back in a centripetal fashion. Where the crests of the reflected and the original wave meet, the pressure inside the vessel is higher than the true pressure in the aorta. This concept explains why the arterial pressure inside the peripheral arteries of the legs and arms is higher than the arterial pressure in the aorta,[21][22][23] and in turn for the higher pressures seen at the ankle compared to the arm with normal ankle brachial pressure index values.
Regulation
The endogenous regulation of arterial pressure is not completely understood. Currently, three mechanisms of regulating arterial pressure have been well-characterized:
- Baroreceptor reflex: Baroreceptors in various organs can detect changes in arterial pressure, and adjust the mean arterial pressure by altering both the force and speed of the heart's contractions, as well as the total peripheral resistance.
- Renin-angiotensin system (RAS): This system is generally known for its long-term adjustment of arterial pressure. This system allows the kidney to compensate for loss in blood volume or drops in arterial pressure by activating an endogenous vasoconstrictor known as angiotensin II.
- Aldosterone release: This steroid hormone is released from the adrenal cortex in response to angiotensin II or high serum potassium levels. Aldosterone stimulates sodium retention and potassium excretion by the kidneys. Since sodium is the main ion that determines the amount of fluid in the blood vessels by osmosis, aldosterone will increase fluid retention, and indirectly, arterial pressure.
These different mechanisms are not necessarily independent of each other, as indicated by the link between the RAS and aldosterone release. Currently, the RAS system is targeted pharmacologically by ACE inhibitors and angiotensin II receptor antagonists. The aldosterone system is directly targeted by spironolactone, an aldosterone antagonist. The fluid retention may be targeted by diuretics; the antihypertensive effect of diuretics is due to its effect on blood volume. Generally, the baroreceptor reflex is not targeted in hypertension because if blocked, individuals may suffer from orthostatic hypotension and fainting.
Pathophysiology
High arterial pressure
The diagnosis of abnormalities in arterial pressure may require serial measurement. Since arterial pressure varies throughout the day, measurements should be taken at the same time of day to ensure the readings taken are comparable. Suitable times are:
- immediately after awakening (before washing/dressing and taking breakfast/drink), while the body is still resting,
- immediately after finishing work.
It is sometimes difficult to meet these requirements at the doctor's office; also, some patients become nervous when their arterial pressure is taken at the office, causing readings to increase (this phenomenon is called white coat hypertension). Taking blood pressure levels at home or work with a home blood pressure monitoring device may help determine a person's true range of arterial pressure readings and avoid false readings from the white coat hypertension effect. Long term assessments may be made with an ambulatory blood pressure device that takes regular arterial pressure readings every half an hour throughout the course of a single day and night.
Aside from the white coat effect, arterial pressure readings outside of a clinical setting are usually slightly lower in the majority of people. The studies that looked into the risks from hypertension and the benefits of lowering the arterial pressure in affected patients were based on readings in a clinical environment.
Arterial pressure exceeding normal values is called arterial hypertension. In itself it is only an acute problem; see hypertensive emergency. But because of its long-term indirect effects (and also as an indicator of other problems) it is a serious worry to physicians diagnosing it.
All levels of arterial pressure put mechanical stress on the arterial walls. Higher pressures increase heart workload and progression of unhealthy tissue growth (atheroma) that develops within the walls of arteries. The higher the pressure, the more stress that is present and the more atheroma tend to progress and the heart muscle tends to thicken, enlarge and become weaker over time.
Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure, arterial aneurysms, and is the leading cause of chronic renal failure. Even moderate elevation of arterial pressure leads to shortened life expectancy. At severely high pressures, mean arterial pressures 50% or more above average, a person can expect to live no more than a few years unless appropriately treated.[24]
In the past, most attention was paid to diastolic pressure; but nowadays it is recognised that both high systolic pressure and high pulse pressure (the numerical difference between systolic and diastolic pressures) are also risk factors. In some cases, it appears that a decrease in excessive diastolic pressure can actually increase risk, due probably to the increased difference between systolic and diastolic pressures (see the article on pulse pressure).
Low arterial pressure
Blood pressure that is too low is known as hypotension. The similarity in pronunciation with hypertension can cause confusion.
Low arterial pressure may be a sign of severe disease and requires urgent medical attention.
When arterial pressure and blood flow decrease beyond a certain point, the perfusion of the brain becomes critically decreased (i.e., the blood supply is not sufficient), causing lightheadedness, dizziness, weakness and fainting.
However, people who function well, while maintaining low arterial pressures have lower rates of cardiovascular disease events than people with normal arterial pressures.
Influential factors
The physics of the circulatory system, as of any fluid system, are very complex. That said, there are many physical factors that influence arterial pressure. Each of these may in turn be influenced by physiological factors, such as diet, exercise, disease, drugs or alcohol, obesity, excess weight and so-forth.
| In cardiac physiology, the rate and volume of flow are accounted for in a combined fashion by cardiac output which is the heart rate (the rate of contraction) multiplied by the stroke volume (the amount of blood pumped out from the heart with each contraction). It represents the efficiency with which the heart circulates blood throughout the body. |
Some physical factors are:
- Rate of pumping. In the circulatory system, this rate is called heart rate, the rate at which blood (the fluid) is pumped by the heart. The higher the heart rate, the higher (potentially, assuming no change in stroke volume) the arterial pressure.
- Volume of fluid or blood volume, the amount of blood that is present in the body. The more blood present in the body, the higher the rate of blood return to the heart and the resulting cardiac output. There is some relationship between dietary salt intake and increased blood volume, potentially resulting in higher arterial pressure, though this varies with the individual and is highly dependent on autonomic nervous system response.
- Resistance. In the circulatory system, this is the resistance of the blood vessels. The higher the resistance, the higher the arterial pressure. Resistance is related to size (the larger the blood vessel, the lower the resistance), as well as the smoothness of the blood vessel walls. Smoothness is reduced by the buildup of fatty deposits on the arterial walls. Substances called vasoconstrictors can reduce the size of blood vessels, thereby increasing blood pressure. Vasodilators (such as nitroglycerin) increase the size of blood vessels, thereby decreasing arterial pressure. Some types of omega-6 fatty acids, particularly from olive oil, have been known to increase vascular smoothness.
- Viscosity, or thickness of the fluid. If the blood gets thicker, the result is an increase in arterial pressure. Certain medical conditions can change the viscosity of the blood. For instance, low red blood cell concentration, anemia, reduces viscosity, whereas increased red blood cell concentration increases viscosity. Viscosity also increases with blood sugar concentration—visualize pumping syrup. It had been thought that aspirin and related "blood thinner" drugs decreased the viscosity of blood, but studies found[25] that they act by reducing the tendency of the blood to clot instead.
In practice, each individual's autonomic nervous system responds to and regulates all these interacting factors so that, although the above issues are important, the actual arterial pressure response of a given individual varies widely because of both split-second and slow-moving responses of the nervous system and end organs. These responses are very effective in changing the variables and resulting blood pressure from moment to moment.
Low arterial pressure
Sometimes the arterial pressure drops significantly when a patient stands up from sitting. This is known as orthostatic hypotension (postural hypotension); gravity reduces the rate of blood return from the body veins below the heart back to the heart, thus reducing stroke volume and cardiac output.
When people are healthy, the veins below their heart quickly constrict and the heart rate increases to minimize and compensate for the gravity effect. This is carried out involuntarily by the autonomic nervous system. The system usually requires a few seconds to fully adjust and if the compensations are too slow or inadequate, the individual will suffer reduced blood flow to the brain, dizziness and potential blackout. Increases in G-loading, such as routinely experienced by acrobatic jet pilots "pulling Gs", greatly increases this effect. Repositioning the body perpendicular to gravity largely eliminates the problem.
Other causes of low arterial pressure include:
- Sepsis
- Hemorrhage - blood loss
- Toxins including toxic doses of blood pressure medicine
- Hormonal abnormalities, such as Addison's disease
Shock is a complex condition which leads to critically decreased perfusion. The usual mechanisms are loss of blood volume, pooling of blood within the veins reducing adequate return to the heart and/or low effective heart pumping. Low arterial pressure, especially low pulse pressure, is a sign of shock and contributes to and reflects decreased perfusion.
If there is a significant difference in the pressure from one arm to the other, that may indicate a narrowing (for example, due to aortic coarctation, aortic dissection, thrombosis or embolism) of an artery.
Venous pressure
Venous pressure is the vascular pressure in a vein or in the atria of the heart. It is much less than arterial pressure, with common values of 5 mmHg (0.7 kPa) in the right atrium and 8 mmHg (1 kPa) in the left atrium. Measurement of pressures in the venous system and the pulmonary vessels plays an important role in intensive care medicine but requires an invasive central venous catheter.the pressure
See अल्सो
"Do You Want To Cure Your Irritable Bowel SyndromeAnd Eat Whatever Healthy Delicious
Foods You Like? Read On!"
Do You Have Irritable Bowel Syndrome and Don't Know What You Should Be Eating?
I have written extensively about Irritable Bowel Syndrome for the last 5 years having overcome my own health problems. During the course of this my readers have constantly been asking me about the diet and what to eat. Now with the help of the U.K.'s top nutritionist and expert in detoxing and a chef with mouth watering delicious recipes I have a recipe ebook for you all to enjoy.
The detox that I did (see link at the bottom of this page) had a massive effect and completely turned my health around. By following a low carb - low glycemic diet you will allow the body to burn off fats cells and release the toxins that are overloading your immune system.
Start Eating The Right Delicious Food And Cure Your I.B.S.
I recommend low glycemic index (G.I.) foods which are slow sugar releasing for a simple reason: It was exactly how nature intended us to eat. Our hormonal systems (incl. the insulin/glycogen axis) have evolved over millions of years. Consumption of sugar rich foods (carbohydrates) and easy access combined with a sedentary lifestyle has resulted in the number of people suffering from I.B.S. to reach epidemic levels in pratically every Westernised Country in the last 25 years.
Why?
Because We're Eating Too Many of the Wrong Type of Carbs and Not Enough Protein!
The building blocks of life are made up of Proteins. Your diet may not be sufficiently high in protein intake - amino acids from proteins like fish (organically sourced or wild) and meat and nuts etc are the building blocks of the body - not carbohydrates like bread, pasta and pastries.
High carb foods such as sugar, alcohol, grains like bread and some fruits feed pathogens like parasites, yeasts, bad bacteria and viruses. Stop feeding these pathogens in your gut and start to improve your health.
By making changes to your diet you can:
1) Start to naturally detox, increasing your glutathione levels (this is your bodies own natural and very powerful detoxifier).
2) Alter the bacterial balance of your gastrointestinal tract which will reduce the number of bad bacteria in your gut and improve digestion resulting in proper breakdown of foods.
3) Burn off fats cells that store toxins.
I know from years of experience and feedback that it's NOT the foods that we eat that are to blame for I.B.S.!
Stop "managing" your I.B.S. and start getting into the mindset of beating it by altering the environment that allows pathogens like bad bacteria and yeast to have free reign.
Food is a powerful drug - Start eating the right types of delicious foods and start feeling the difference in your well-being!


